
Can You Get Pregnant During Menopause? Understanding the Possibilities
Introduction Menopause marks the end of a woman’s reproductive years, typically occurring between 45-55 years of age. However, many women wonder: Can you still get

Introduction Menopause marks the end of a woman’s reproductive years, typically occurring between 45-55 years of age. However, many women wonder: Can you still get
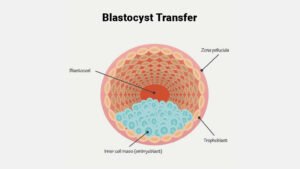
Introduction IVF treatments are advancing rapidly, with new techniques improving success rates. One such technique is embryo pooling, a process where embryos from multiple IVF

Introduction Thyroid hormones play a crucial role in regulating various bodily functions, including metabolism, energy levels, and reproductive health. An imbalance in these hormones can

Introduction Often left helpless, many couples struggling with infertility have to rely on fertility clinics. REVIVA IVF and Fertility Clinic in Chandigarh, has gained some

How does it affect fertility? Endocrine Assessment- Hormone tests were carried out as part of the first examination of women seeking reproduction treatment is known

In this blog, we will take a close look at the DNA fragmentation test of sperm and how helpful it is in determining male fertility.

Our breakthrough is preimplantation genetic screening (PGT-A) of embryos for abnormalities. #PGT offers voluble insights into the genetic composition of embryos Helping couples make informed

Your fallopian tubes play a vital role in the fertilization process necessary to become pregnant. These tubes are where the egg & sperm meet &
With the aid of ART, such as IVF, infertile intended parents can have children. We have come up with the best and easiest solution for

Ovulation occurs when the ovary releases an egg and some women experience bleeding & spotting around the time they are ovulating, which is a normal

Recurrent Implantation Failure (RIF) Recurrent implantation failure refers to the inability of embryos to implant into the uterine lining after repeated attempts at
If you want to get pregnant and you are diagnosed with endometriosis, you might assume that all hope is lost. With the right treatment, you




Monday to Saturday: 9:00am – 5:00pm
© 2020-24 REVIVA IVF. All right reserved. | Sitemap
WhatsApp us
WhatsApp us